Why Did My Patient “Pass Out”?
Written by Bryan Cardiologist John Steuter, MD
Syncope is a clinical syndrome in which transient loss of consciousness (TLOC) is caused by a period of inadequate cerebral flow. Typically the period of time with inadequate cerebral flow is relatively brief and, by definition, self-limited. It is often the result of cerebral hypo-perfusion due to transient hypotension.
Causes and Conditions of TLOC and Syncope
The possible causes of TLOC resulting in true syncope are generally grouped into four major categories, including:
- Reflex (neurally-mediated) syncope
- Orthostatic syncope
- Cardiac arrhythmias
- Structural cardiopulmonary disease
Conditions that mimic TLOC/syncope but are not true syncope include:
- Seizures
- Sleep disturbances
- Accidental falls
- Some psychiatric conditions
Identifying Syncope
For nearly all patients, the initial evaluation of suspected syncope should include obtaining a comprehensive history, performing a physical examination and review of an electrocardiogram. While not all encompassing, certain patient characteristics and symptoms can help delineate the etiology as noted below.
Syncope due to orthostatic hypotension:
- Passes out after standing up
- Passes out after prolonged standing especially in crowded, hot places
- Temporal relationship with start or changes of dosage of vasodepressive drugs leading to hypotension
- Presence of autonomic neuropathy or Parkinsonism
Neurally mediated syncope:
- Absence of heart disease
- Long history of recurrent syncope after sudden unexpected unpleasant sight, sound, smell or pain
- Nausea or vomiting associated with syncope with head rotation or pressure on carotid sinus (as in shaving, tight collars)
Cardiovascular syncope:
- Presence of definite structural heart disease
- Family history of unexplained sudden death or channelopathy, during exertion or supine
- ECG findings suggesting arrhythmic syncope (non-sustained ventricular tachycardia (VT), bifascicular block (defined as either LBBB or RBBB combined with left anterior or left posterior fascicular block)
- Asymptomatic inappropriate sinus bradycardia (<50 bpm), sinoatrial block or sinus pause ≥3 s in the absence of negatively chronotropic medications, long or short QT intervals)
- Sudden onset palpitation immediately followed by syncope
Syncope or Not? Identifying Risk
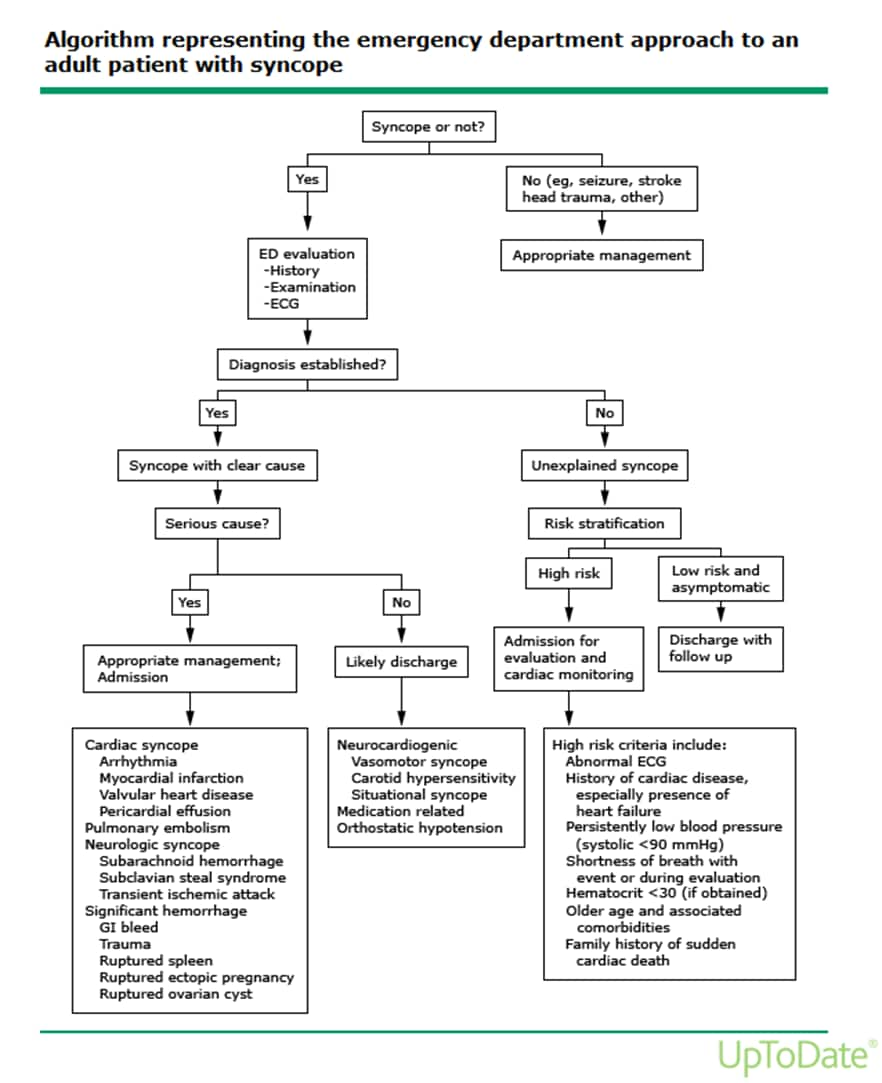
Risk stratifying these patients can be difficult but the algorithm below can provide practitioners with guidelines.
Evaluating Syncope
If you have a patient who is experiencing possible symptoms of syncope, or would like further information on evaluating a patient who could be at risk, contact Bryan Heart at 402-483-3333.

